By now, healthcare workers are keenly aware of the recommendations regarding use of traditional nail polish and artificial nails by healthcare workers and workers who are employed in patient care areas. The evidence and guidelines support not wearing artificial nails and either not using nail polish or ensuring the polish is intact. Most hospitals have adopted policies to that effect.
With the newer gel polish products being widely available, many nurses utilize this longer lasting “polish” that stays intact for longer than traditional polish. But...is it safe?
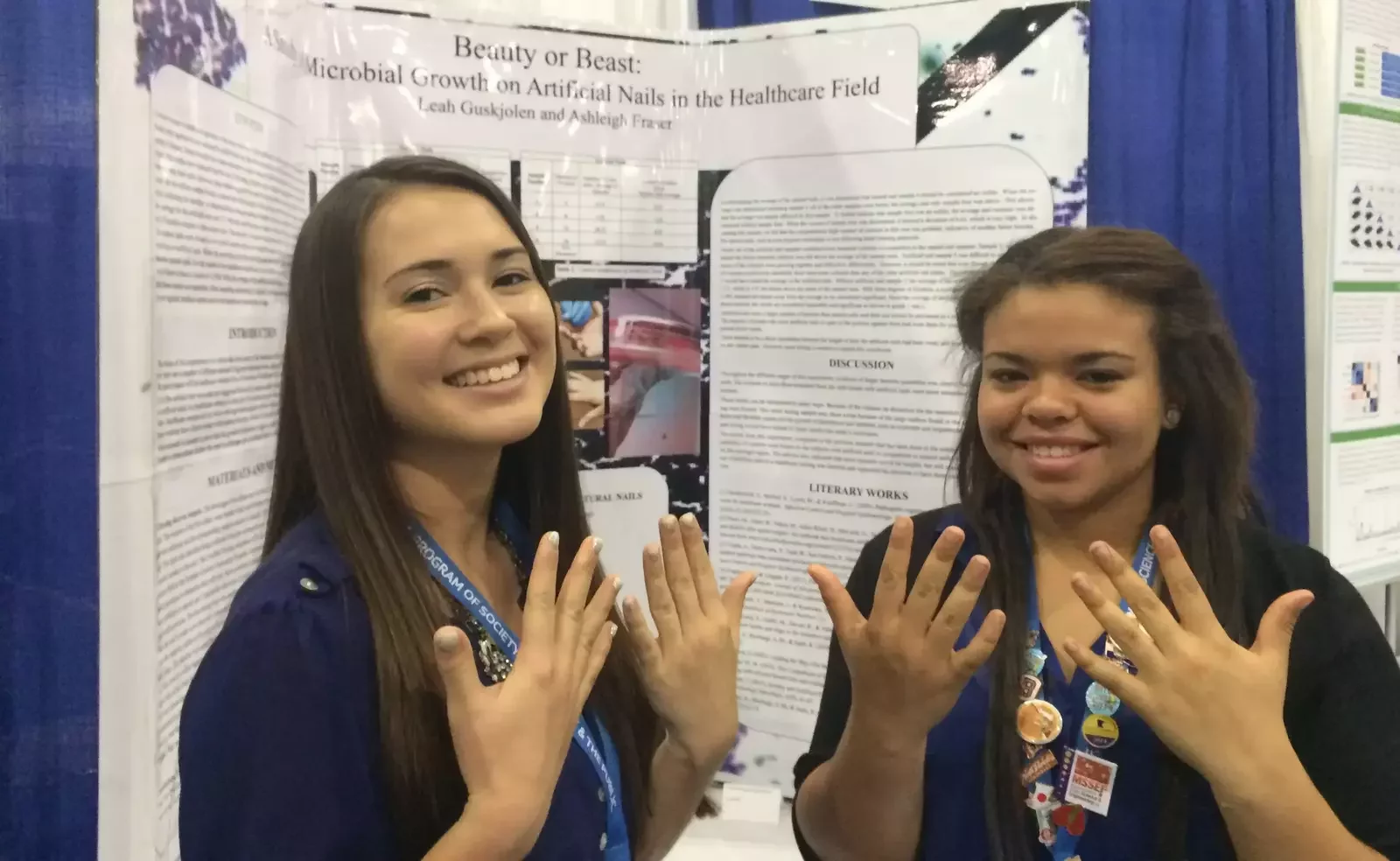
The Association of Operating Room Nurses (AORN) recently made a position statement on the use of gel polish in operating rooms that asserts that gel polish not be worn in these areas. The rationale is that very few studies have been done and evidence doesn’t support its safe use. {1} The Association for Professionals in Infection Control and Epidemiology (APIC) endorses this statement. {2}
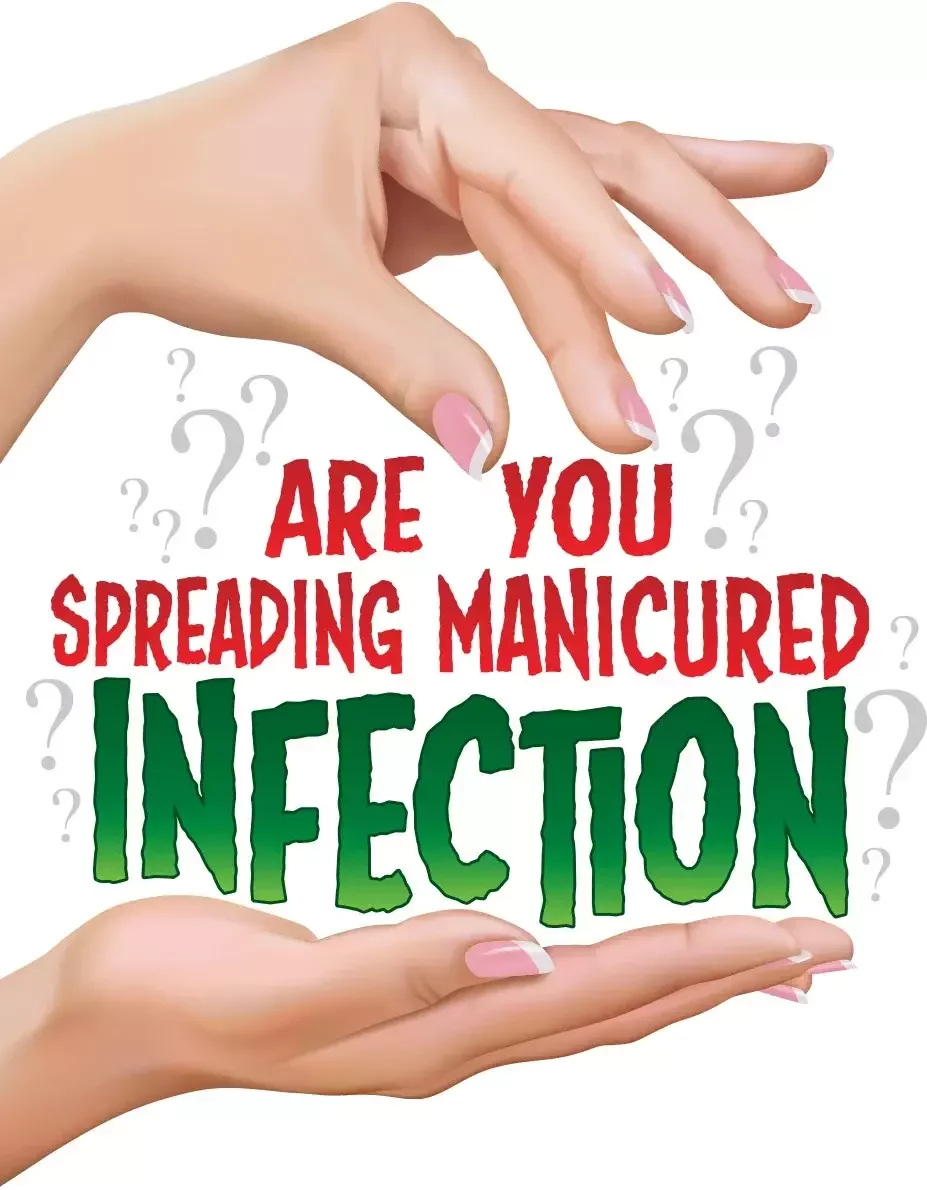
The World Health Organization (WHO) states that HCWs who wear artificial nails are more likely to harbor Gram-negative pathogens on their fingertips than those who have natural nails, both before and after hand washing or hand rub with an alcohol-based gel. Additionally, the WHO recommends that HCWs do not wear artificial fingernails or extenders when having direct contact with patients and that natural nails should be kept short. {3}
The CDC concurs with the WHO and recommends keeping natural nails short: less than ¼-inch long. {4} The Society for Healthcare Epidemiology of America (SHEA) & Infectious Diseases Society of America (IDSA) state that, based on a lack of evidence on gel nails specifically, a conservative approach (treating them as artificial nails) should be considered. If this is the case, then at the very least, gel nails should not be worn in high infection-risk areas. {5}

Based on evidence and recommendations, some hospitals are going to a “clean, short, natural nails” policy for all patient care area workers. Given the lack of hospital hand hygiene adherence (as low as 40-50%) {6}, the increased risk of artificial and chipped nail polish harboring bacteria, and the high potential for hospital acquired infection, this stringent approach to nail grooming may be impactful in reducing potential of spreading infection.
1: http://www.aorn.org/guidelines/clinical-resources/clinical-faqs/hand-antisepsis-hygiene#gelshellac (link no longer available)
2. http://www.apic.org/Professional-Practice/Practice-Resources
3: http://apps.who.int/iris/bitstream/10665/44102/1/9789241597906_eng.pdf
4. http://www.cdc.gov/mmwr/PDF/rr/rr5116.pdf
5. Ellingson, K., Haas, J. P., Aiello, A. E., Kusek, L., Maragakis, L. L., Olmsted, R. N., & ... Yokoe, D. S. (2014). Strategies to Prevent Healthcare-Associated Infections through Hand Hygiene. Infection Control & Hospital Epidemiology, 35(8), 937-960. doi:10.1086/677145 http://www.jstor.org/stable/10.1086/677145
6: Improving Hand Hygiene at Eight Hospitals in the United States by Targeting Specific Causes of Noncompliance. (2015). The Joint Commission Journal on Quality and Patient Safety, 41(1), 4-12. Retrieved August 7, 2015, from https://pubmed.ncbi.nlm.nih.gov/25976719/