Isn’t it time that we do something about this?
What does your facility do with its Event and Incident data? Is the data at least somewhat transparent throughout your organization and are you a part of the action being taken to correct issues?

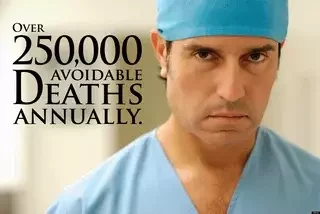
Take a moment to refresh yourself on which events qualify as “Serious Reportable Events.”
List of the “SRE”s from the NQF 2006 Update:
In order to assist in this effort, the list of “Serious Reportable Events” (SREs) was developed so that process failures could be identified and remedied and to create public accountability for adverse events incurred in the delivery of health care (1).
Many of the events listed above are conditions included in the Joint Commission core measures and in the CMS Hospital Acquired Condition Reduction Program (1), which demonstrates these are indeed national issues and action needs to immediately be taken to improve the numbers.
Keep in mind that even the Joint Commission only has a voluntary reporting system for what it deems as Sentinel Events (SE), so the data released on SEs is highly inaccurate.

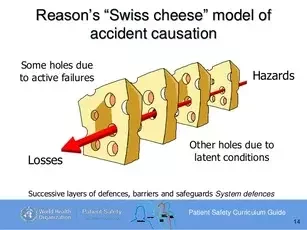
- Are you aware of any medical events or incidents that have recently occurred?
- What about the details of the event?
- Is transparency recognized and embraced so even your front-line staff is aware of any near-misses?
- Does Quality & Risk determine the root cause and present their determinations/report to all staff as a learning exercise?
- Do processes improve and change as a result?

Credits:
1) http://www.ahrq.gov/downloads/pub/advances/vol4/kizer2.pdf
2) http://www.qualityforum.org/Publications/2007/03/Serious_Reportable_Events_in_Healthcare–2006_Update.aspx (download publication)
3) Patient Safety Map & Toolkit. (2009, August 31). Retrieved from National Academy for State Health Policy: http://www.nashp.org/patient-safety-toolkit/
4) Study Suggests Medical Error Now Third Leading Cause of Death in the U.S. (2016, May 3). Retrieved from Johns Hopkins Medicine: http://www.hopkinsmedicine.org/news/media/releases/study_suggests_medical_errors_now_third_leading_cause_of_death_in_the_us